Hi Everyone, welcome to my first blog on our new website!
This blog discusses Developmental Coordination Disorder (DCD), which may be an appropriate diagnosis for some children with difficulties attaining/performing motor skills.
Today I thought I’d discuss the children who are referred to Therapies For Kids who are described as:
- Being clumsy
- Needing help keeping up with peers with sports, tying shoe laces, doing buttons, struggling with handwriting, etc.
- Frequent falls
- Delays in developing specific motor skills, e.g bike riding, ball catching, and sporting skills etc.
- They may have difficulty with coordination of both sides of their body
- Difficulty with handwriting
- Has poor balance

How is DCD diagnosed?
It is a condition recognised officially by the World Health Organization and diagnosed using a tool known as the DSMV. DCD needs to be officially diagnosed by a medical practitioner. This can be a paediatrician/neurologist/psychologist. To get a diagnosis of DCD, the child has to demonstrate the following:
- Marked impairment of the development of motor coordination.
- The coordination difficulties cannot be due to any recognised neurological condition.
- Motor difficulties significantly interfere with ADLs (activities of daily living), academic achievement, social participation etc. (APA, 2000)
Does DCD occur alone?
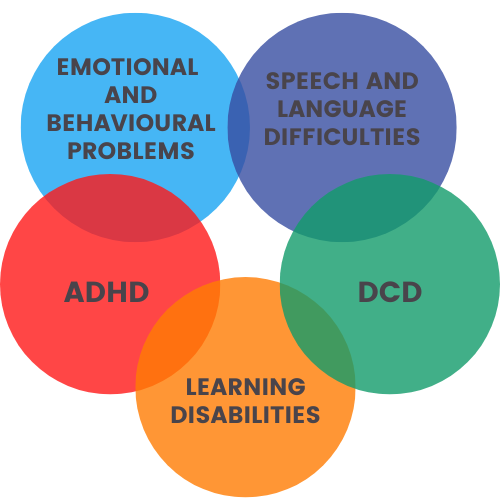
DCD is often more than a motor problem. At least half of all children with DCD have attention deficit hyperactivity disorder(ADHD), and many have learning disabilities. In addition, DCD is much more common in children born preterm and children with autism.
Do children with DCD “outgrow” motor difficulties?
Research shows us that DCD persists throughout adolescence and into adulthood. Children with DCD do learn motor tasks; however, they have difficulty when faced with new age-appropriate skills, even when they’ve mastered younger skills.

Role of therapy for children with DCD
Early therapy intervention has been found to be beneficial for children with DCD.
Occupational therapy and physiotherapy have historically been the therapies of choice. All therapists (such as physiotherapists and occupational therapists) are educated and trained in looking at motor skills and where the child struggles to perform that skill. In addition, in consultation with carers, we at Therapies For Kids will assist you in determining your child’s ability to cope with the demands and activities of daily life.
Therapy can assist with the following:
- The acquisition of motor skills
- Motor planning and coordination
- Activities of daily living
- Working memory
- Fine motor skills in the classroom
Therapy may also help reduce emotional, physical and social issues that are common in children with DCD.
At Therapies For Kids, we know that children with DCD may also have language/oral motor issues and need to see a Speech Pathologist as well; therefore, we may refer you for an assessment by one of our Speech Pathologists.

How do we assess children who present difficulties with motor skills at Therapies For Kids?
On referral to Therapies For Kids, you may choose to see one or more of our therapists to assess where your child is functioning compared to their peers and the impact it is having on their development and performance of skills. Firstly you will be asked questions about your child’s:
- Physical skills - gross motor, fine motor, pro motor
- Whether they avoid certain activities, i.e. social /physical participation
- How they are performing at school etc
Physiotherapists will look primarily at motor activities e.g.:
- Gross motor skills and coordination
- Motor planning (ability to carry out a skilled motor activity)
- Ability to balance
- Ability to perform ball skills
- Ability to do activities that increase gross motor skills
An Occupational Therapist will look at the following:
- Activities of daily living, e.g. using utensils (knife and fork)
- Handwriting, using scissors
- Ability to do multi-step activities
- Ability to play complex games
- Sensory processing of information used to perform tasks
A Speech Pathologist will help assess if your child has the following:
- Difficulty with saying sounds and correct articulation
- Whether they jumble words
- Have difficulty with short-term memory
- Social and emotional difficulties
How do you get a diagnosis of DCD for your child?
Once your therapists have gathered information on your child’s motor performance, they will refer you to your GP for a referral to the appropriate medical practitioner. Your child will then be assessed to make sure there is no underlying neurological cause. Then with the information given by your child’s therapist/ teacher etc, they can advise if DCD is an appropriate diagnosis.

What can we do to help?
- Your therapist will work with you to develop goals to improve your child's functional skills
- Activity-based goals - specific tasks - ADL/ handwriting etc
- A problem-solving approach to work through challenging activities
- Education for parents to help children with DCD
- Accommodations/ adaptations in their daily life
- Co-op approach (cognitive orientation to daily occupational performance)
- Child-centred performance-based approach
- Goal-directed training: the importance of setting goals
In Physiotherapy, your therapist may work on some or all of the following:
- Core stability
- Tasks oriented skills
- Balance skills
- Complex skills with multi-directional components, e.g. ball and bat, star jumps, bike riding, skipping with a rope, using a swing
- Motor skills, i.e. hopping, jumping, running
- Motor planning
- Processing speed
- Crossing midline activities
- Treat specific motor issues
In Speech Pathology, your therapist may work on some or all of the following:
- Improving motor control
- Improve motor patterns of speech
- May focus on producing specific sounds or words and phrases of difficult lengths
- Increasing vocabulary is limited
- Provide a supportive environment for practising language skill
In Occupational Therapy, your therapist may work on some or all of the following:
- Activity-based goals - specific tasks - ADL/ handwriting etc
- A problem-solving approach to work through challenging activitie
- Practise produce
- Education for parents to help children with DCD
- Accommodations/adaptions
- Co-op approach (cognitive orientation to daily occupational performance)
- Child-centred performance-based approach
- Goal-directed training- the importance of setting goal
- Assistive Technology/WI/Lusiomate
- Allow processing time

Frequently Asked Questions
What is the difference between DCD and dyspraxia?
These two terms are often used interchangeably when discussing children with motor coordination difficulties. However, DCD is the formal term, and dyspraxia is not. Dyspraxia is used in many different ways, unlike DCD, as there are no formal criteria.
Can treatment cure my child?
There is no cure for DCD, but with early intervention and therapy, children can learn strategies to compensate for their coordination difficulties. Therapy breaks tasks down so they can learn the steps to acquire motor skills.
What can I do to help my child?
- Get an assessment of your child's motor skills by a therapist
- Seek a formal diagnosis from your medical practitioner
- Understand DCD and its impact on your child
- Work with all the professionals involved with your child so that techniques can be used in all situations
What things can I do at home?
- Recognise your child's strengths!
- Encourage your child to participate in physical activities for enjoyment, not competition Introduce physical activity individually before doing it with peers (ie learn the skills/ rules first)
- Use clothes that are easy to get off, e.g. velcro shoes, no buttons or snaps
- Encourage activities at home that involve planning, e.g. unpacking the dishwasher/ shopping/ setting the table